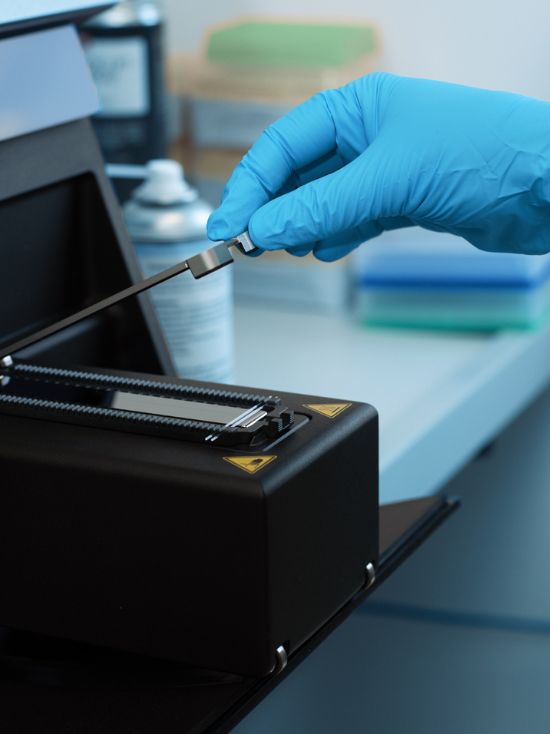
Discover a new way to cure bacterial infections
Your Life
Is Our Priority
Many pathogens are already resistant to antibiotics today. As a result, each year, millions of people lose their life because of bacterial infections.
With your support, we will finally put an end to this incredibly tragic situation – and create a healthier and better future for us all.